Updated Treatment Guidelines for Non-Small Cell Lung Cancer
Non-small cell lung cancer (NSCLC) represents the most prevalent form of lung cancer, comprising about 85% of all lung cancer cases. This article explores the latest treatment guidelines for NSCLC, emphasizing the role of immunotherapy, traditional treatments, and the importance of patient-centered care.
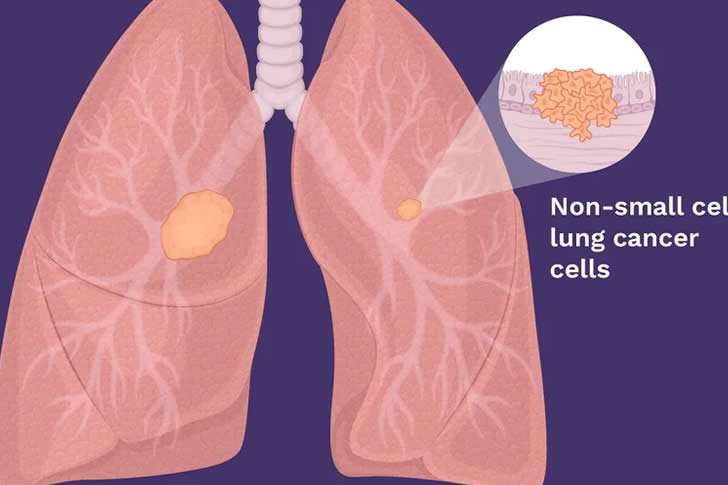
Understanding Non-Small Cell Lung Cancer
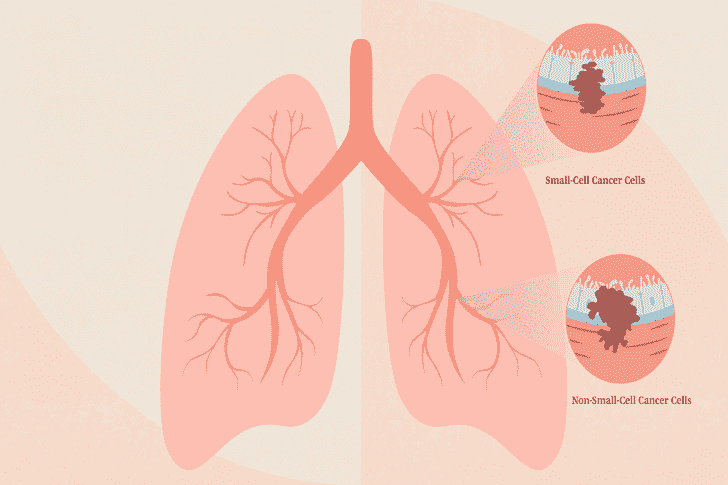
Types and Symptoms of NSCLC
NSCLC is the predominant form of lung cancer, making up approximately 85% of diagnoses. It primarily includes subtypes such as squamous cell carcinoma, adenocarcinoma, and large cell carcinoma. In its early stages, NSCLC may not manifest any symptoms and often gets detected incidentally during routine checks or other medical evaluations. As the cancer advances, symptoms like cough, sputum production, chest pain, shortness of breath, and weight loss can emerge. Additionally, complications such as bone pain from metastasis or neurological symptoms from brain metastasis might occur.
Diagnostic Techniques
The following methods are commonly employed to diagnose NSCLC:
- Chest X-ray and CT Scan: Essential for initial tumor detection.
- Pathological Biopsy: Crucial for determining the type and stage of cancer.
- Advanced Imaging: Includes PET/CT and MRI scans to thoroughly assess the extent of the disease.
The staging of NSCLC, which guides prognosis and treatment strategy, depends on tumor size, lymph node involvement, and the presence of distant metastases as summarized in the table:
| Stage | Tumor Size | Lymph Node Involvement | Metastasis | Prognosis |
|---|---|---|---|---|
| Early | Small | No | No | Favorable |
| Advanced | Large | Yes | Yes | Poor |
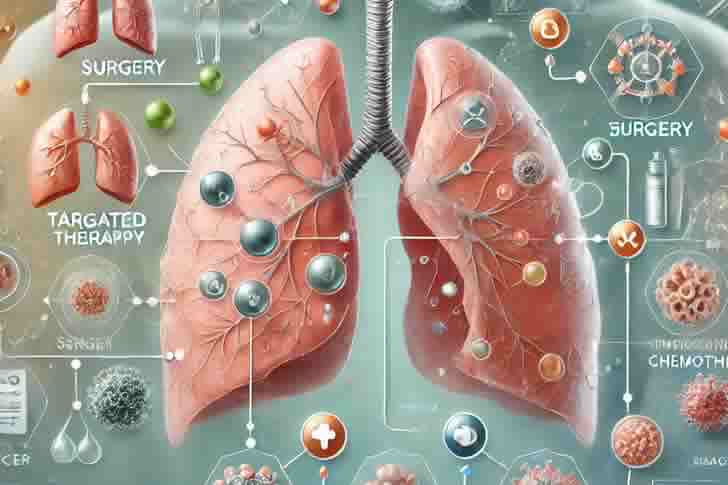
The Role of Immunotherapy in NSCLC
Immunotherapy marks a significant advancement in NSCLC treatment, particularly for cases where traditional therapies have failed. This treatment modality enhances the body’s immune response against cancer cells.
Key Considerations for Immunotherapy
- Patient Selection: Not every patient with NSCLC is suitable for immunotherapy. Important factors include tumor histology, biomarker status (e.g., PD-L1 expression), and overall health.
- Combination Therapy: Immunotherapy can be administered alone or in combination with other treatments such as chemotherapy or targeted therapy, often leading to improved outcomes but also a higher risk of side effects.
- Monitoring and Management: Continuous monitoring through imaging and blood tests is crucial to assess the treatment’s effectiveness and manage any side effects promptly.
- Side Effects: Although generally well-tolerated, immunotherapy can cause side effects affecting various organs and systems. It’s vital for patients to be aware and report any adverse effects immediately.
Comparing Immunotherapy to Traditional Treatments
Immunotherapy offers several benefits over traditional methods, especially in terms of response rates, survival times, and overall quality of life as detailed:
| Treatment | Response Rates | Long-Term Survival | Quality of Life |
|---|---|---|---|
| Immunotherapy | Higher | Extended | Better |
| Traditional | Lower | Limited | Reduced |
A Focus on Atezolizumab (Tecentriq)
Atezolizumab, a PD-L1 inhibitor, has been a notable development in the immunotherapy space. Approved in 2016 for treating advanced NSCLC, it’s applicable both as a primary and secondary line of treatment.
Efficacy and Usage
- Indications: Suitable for patients with high PD-L1 expression and no previous chemotherapy, or those who have not responded to platinum-based chemotherapy.
- Clinical Outcomes: Proven to significantly improve progression-free and overall survival rates, and it can enhance the objective response rate in subsequent treatments.
Conclusion: Embracing Immunotherapy for Advanced NSCLC
Immunotherapy has transformed the treatment landscape for NSCLC, providing new hope and improved treatment prospects for advanced-stage patients. By adhering to the latest guidelines and collaborating closely with healthcare providers, patients can navigate their treatment options effectively. Active patient involvement and continuous support from the medical team are crucial for achieving the best treatment outcomes. Further research will likely expand the applications and effectiveness of immunotherapy in NSCLC.
https://www.cancer.gov/types/lung/hp/non-small-cell-lung-treatment-pdq
https://emedicine.medscape.com/article/2241676-overview?form=fpf
Non-small cell lung cancer (NSCLC) remains one of the most common types of lung cancer, and treatment options continue to evolve. Updated guidelines offer new insights into how best to manage the disease, depending on its stage, genetic mutations, and patient health. This article reviews four updated treatment approaches for NSCLC, providing guidance on the latest therapies and strategies for improving patient outcomes.








Recent Comments