Evolving Therapies for Non-Small Cell Lung Cancer
Non-small cell lung cancer (NSCLC) is the most common type of lung cancer, accounting for approximately 85% of all lung cancer cases. This article outlines the latest treatment guidelines for NSCLC, focusing on the most recent developments in targeted therapies, immunotherapy, and combination treatments.
Overview of NSCLC
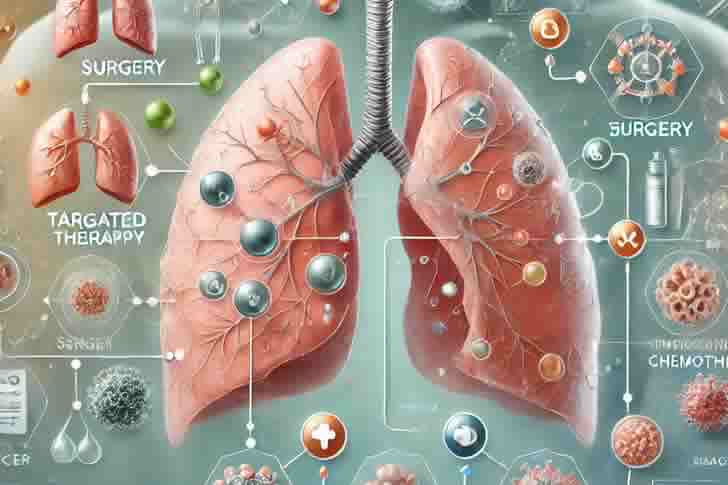
NSCLC encompasses several subtypes, including adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Treatment approaches vary depending on the stage of the cancer, the presence of specific genetic mutations, and the overall health of the patient. The primary goals of treatment are to prolong survival, reduce symptoms, and improve quality of life.
Current Treatment Guidelines
The latest guidelines for treating NSCLC are shaped by the cancer’s stage at diagnosis, the molecular profile of the tumor, and the patient’s overall health and preferences.
1. Early-Stage NSCLC (Stage I-IIIA)
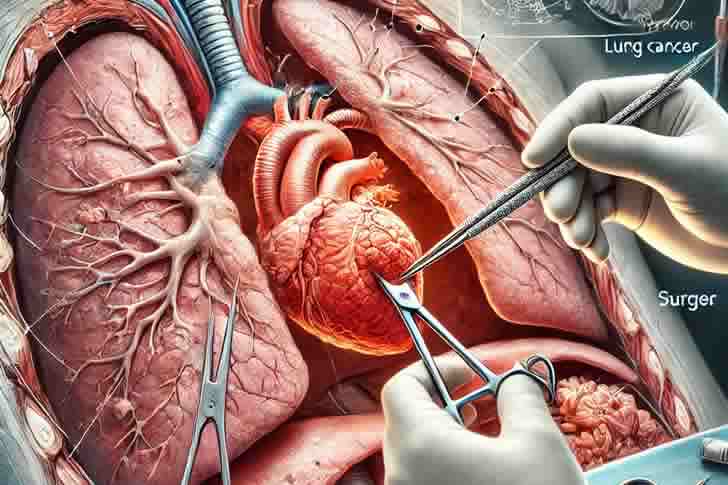
- Surgical Resection: Surgery remains the cornerstone of treatment for patients with early-stage NSCLC. For those who are eligible, a complete surgical resection offers the best chance for a cure.
- Adjuvant Chemotherapy: Following surgery, patients with high-risk features (e.g., large tumors or lymph node involvement) may benefit from adjuvant chemotherapy to reduce the risk of recurrence.
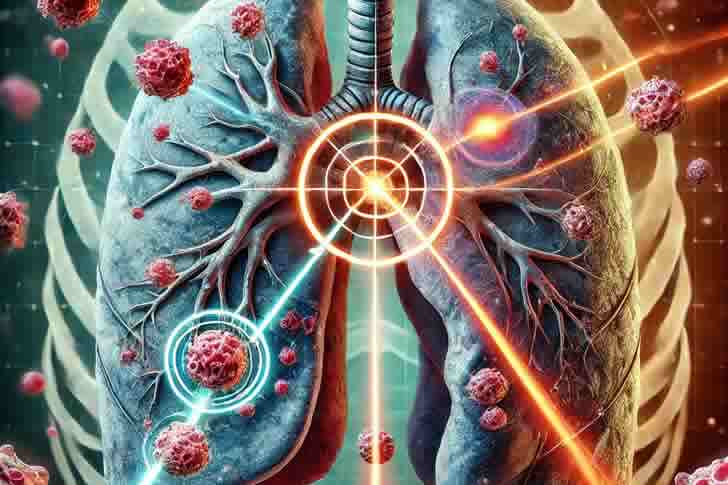
- Radiation Therapy: For patients who are not surgical candidates, radiation therapy, often in combination with chemotherapy, is a standard option.
2. Locally Advanced NSCLC (Stage IIIB)
- Chemoradiation: Concurrent chemotherapy and radiation therapy are recommended for patients with locally advanced NSCLC. This combination aims to control the tumor locally and reduce the likelihood of distant metastasis.
- Immunotherapy: The addition of immunotherapy, particularly durvalumab, after chemoradiation has become a standard approach based on recent clinical trials showing improved progression-free survival.
3. Advanced or Metastatic NSCLC (Stage IV)
- Molecular Testing: All patients with advanced NSCLC should undergo molecular testing to identify actionable genetic mutations (e.g., EGFR, ALK, ROS1, BRAF). These mutations can guide the selection of targeted therapies.
- Targeted Therapies: For patients with specific mutations, targeted therapies such as osimertinib (EGFR), alectinib (ALK), and entrectinib (ROS1) are preferred due to their effectiveness and favorable side effect profiles.
- Immunotherapy: Immune checkpoint inhibitors like pembrolizumab and nivolumab are recommended for patients without targetable mutations, especially if their tumors express PD-L1. These agents can be used alone or in combination with chemotherapy.
- Chemotherapy: For patients ineligible for targeted therapies or immunotherapy, chemotherapy remains a key treatment option, often combined with bevacizumab or other agents.
4. Maintenance Therapy
- Continuation of Therapy: Patients who respond to initial treatment may continue with maintenance therapy to prolong the duration of response. This may involve ongoing use of the initial treatment regimen or a switch to another agent to maintain disease control.
5. Palliative Care
- Symptom Management: Palliative care should be integrated into the treatment plan for all NSCLC patients, regardless of the stage, to manage symptoms and improve quality of life.
- Supportive Therapies: These may include pain management, nutritional support, and psychological counseling to address the holistic needs of the patient.
Key Developments in NSCLC Treatment
- Liquid Biopsy: This non-invasive testing method is increasingly used to detect genetic mutations and monitor treatment response, offering a less invasive alternative to traditional tissue biopsies.
- Combination Therapies: Ongoing research is exploring the benefits of combining immunotherapy with targeted therapies, chemotherapy, or radiation, aiming to enhance treatment efficacy.
- Personalized Medicine: Advances in molecular profiling are driving the move toward personalized treatment plans, where therapies are tailored to the genetic makeup of the individual’s cancer.
Professional Analysis: Treatment Options Comparison
| Treatment Approach | Stage of NSCLC | Benefits | Considerations |
|---|---|---|---|
| Surgery | Early-Stage (I-IIIA) | Potential for cure | Requires sufficient health for surgery |
| Chemoradiation | Locally Advanced (IIIB) | Controls tumor growth, improves survival | Associated with significant side effects |
| Targeted Therapy | Advanced (IV) | Effective for specific mutations | Requires molecular testing, resistance can develop |
| Immunotherapy | Advanced (IV) | Long-term survival benefits in some patients | Response varies based on PD-L1 expression |
| Chemotherapy | All stages | Broad applicability | Side effects include nausea, fatigue, and infection risk |
Frequently Asked Questions (FAQ)
Q1: What are the side effects of immunotherapy in NSCLC?
A1: Common side effects of immunotherapy include fatigue, skin rash, and gastrointestinal issues. In some cases, more serious immune-related side effects can occur, such as pneumonitis, colitis, or hepatitis.
Q2: How do I know if targeted therapy is right for me?
A2: Targeted therapy is suitable for patients whose tumors have specific genetic mutations, such as EGFR, ALK, or ROS1. Molecular testing is essential to determine eligibility for these therapies.
Q3: Can NSCLC be cured?
A3: Early-stage NSCLC can potentially be cured with surgery, especially if the cancer is detected before it spreads. For advanced stages, treatment focuses on prolonging survival and improving quality of life.
Q4: What is the role of maintenance therapy in NSCLC?
A4: Maintenance therapy helps to prolong the effects of the initial treatment by keeping the cancer under control. It is typically used in patients who respond well to initial therapy.
Conclusion
The treatment landscape for non-small cell lung cancer continues to evolve, with new therapies offering hope for improved survival and quality of life. The latest guidelines emphasize the importance of molecular testing to guide treatment decisions, the integration of immunotherapy into standard care, and the ongoing development of personalized treatment plans. As research progresses, these guidelines will continue to adapt, providing patients with the most effective and individualized care possible.
References








Recent Comments